Innovative preclinical studies for neurodegenerative disorders & diseases
Enterosys is a CRO for preclinical studies scientifically rooted in the gut and gut-brain axis
While the idea that the brain can alter gut function has been documented and accepted, the evidence for intestinal signals that affect mood, behavior, cognitive function, or even metabolism… is less known.
The mutual impact that the gastrointestinal tract and brain function have on one another is summarized in the concept of the “gut-brain axis”. Numerous studies of this complex system have highlighted the multiplicity and diversity of the different components of the axis. Experimental studies conducted in recent years have shown that neural circuits have a central (but not unique) role in the connections between the gut and the brain. Hormonal and immunological pathways, as well as the gut microbiota, integrate information at the base of a complex network. Its dysfunction can have pathophysiological consequences, as it not only influences gastrointestinal efficiency but also modulates central functions.
Neurologic disorders & diseases interacting with the gut and gut-brain axis
AGING
As we age, both the immune system and the gut microbiome undergo significant changes in composition and function that are correlated with an increased susceptibility to diseases.
ALZHEIMER’S DISEASE
Alzheimer’s diseases leads to dementia. Emerging evidence suggests a relationship between the gut microbiota, brain health and the risk of developing this disease.
AUTISM
Autism spectrum disorders (ASD) are associated with the dysregulation of the microbiota-gut-brain axis, and changes in microbiota composition.
DEPRESSION
Clinical depression or major depressive disorder (MDD) is a common mental illness. Evidence suggests that the gut microbiota and bidirectional communication axis between the gastrointestinal tract and the brain play an essential role in regulating brain functions and the pathogenesis of neuropsychiatric diseases.
EPILEPSY
Recently, evidence has emerged that a dysbiosis in the gut may be associated with certain forms of epilepsy. The link between gut microbiota and brain may explain epilepsy.
MULTIPLE SCLEROSIS
Multiple sclerosis (MS) is an inflammatory demyelinating disease of the central nervous system (CNS), the etiology of which is still unclear, albeit believed to result from an autoimmune attack on CNS components.
PARKINSON’S DISEASE
Increasing evidence suggests that Parkinson’s disease (PD) starts in the gut, with retrograde transmission of misfolded alpha-synuclein spreading from the enteric nervous system (ENS) to higher brain centers along vagal afferents.
PSYCHOLOGICAL STRESS
Stress alters the activity of the gut-brain axis, potentially causing intestinal barrier dysfunction, which in turn induces cognitive and mood impairments through exacerbated inflammation.
At the cutting edge of preclinical studies for neurologic diseases
There is growing evidence of the impact of the gut microbiota on the gut-brain axis and the ensuing repercussions on health and disease. A stable gut microbiota is essential for normal gut physiology and contributes to appropriate signaling along the gut-brain axis and, thereby, to the healthy status of the individual.
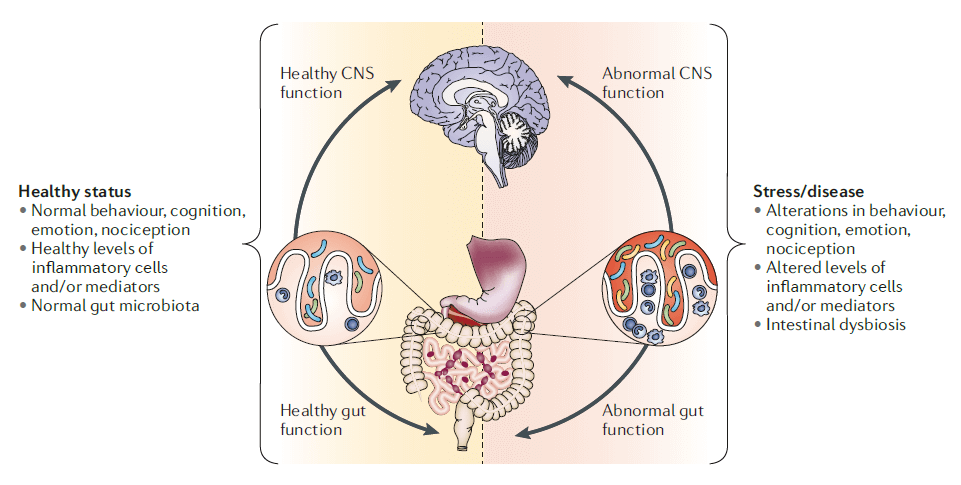
Figure from Cryan JF, Dinan TG. Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour. Nat Rev Neurosci. 2012 Oct;13(10):701-12. doi: 10.1038/nrn3346. Epub 2012 Sep 12. PMID: 22968153.
Discover our preclinical models
Enterosys offers you a complete and innovative range of preclinical protocols based on in vitro and in vivo efficacy tests.
Discover our approach
Our experience in R&D and our innovative management approach allow us to provide support in the design and development of new models in order to meet your objectives.
Discover our preclinical models
Enterosys offers you a complete and innovative offer of preclinical protocols based on in vitro and in vivo efficacy tests.
Discover our approach
Our experience in R&D allows us to meet your objectives and offer you support for the design and development of new models, guided by our innovation management approach.
Gut & gut-organ communication: a major role in many disorders and diseases
GASTROINTESTINAL DISEASES
METABOLIC
DISEASES
DERMATOLOGICAL DISEASES
Do you have a question about the contribution of gut models in your innovative research ?
Our team of experts will be delighted to answer all of your questions. We guide you in the design of an optimized protocol to meet your objectives and add value to your molecules with quick and concrete solutions.